
Publié il y a 4 mois
26.11.2025
Partager
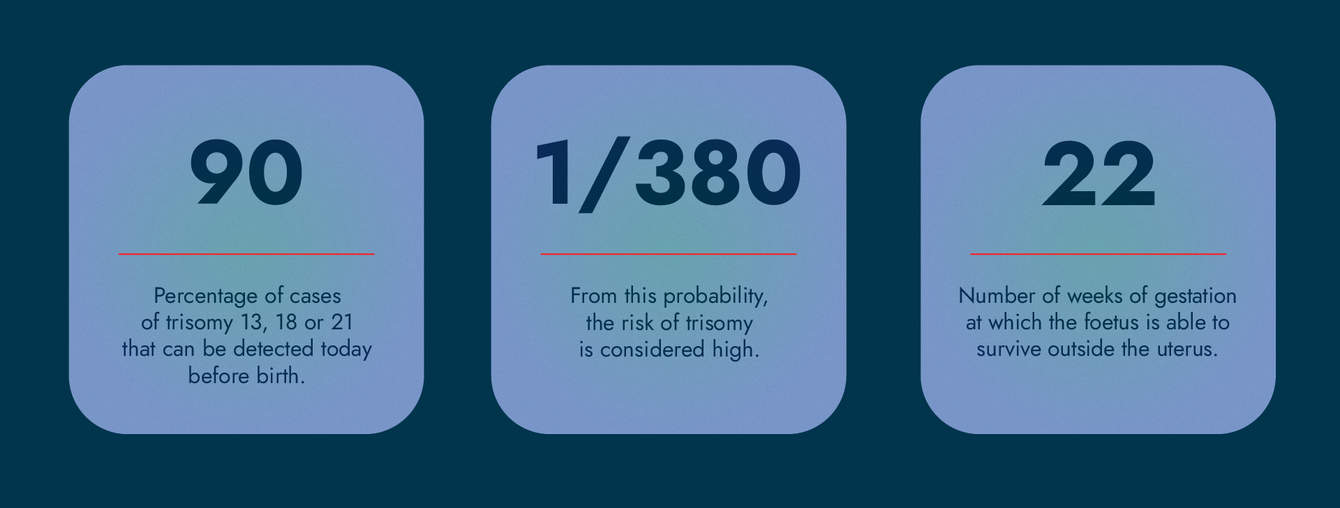
“Before the 1990s, many mothers, especially those over the age of 35 years, were advised to undergo amniocentesis, a procedure that involves collecting amniotic fluid from the uterus using a fine needle,” notes Dr Joanna Sichitiu, in charge of the Ultrasound Unit at the CHUV. “The new generation now benefits from less invasive prenatal screening.” Thus, more than 90% of cases of trisomy 13, 18 or 21 can be detected before birth. Other tests can detect certain congenital malformations or risks of preeclampsia, a complication affecting 2% of pregnancies. Prenatal diagnosis provides parents with more information about the child's quality of life. It allows the medical team to organise the best possible follow-up for the mothers concerned and their foetus during pregnancy and childbirth. It is, of course, carried out with the consent of the pregnant person.
The Key First-Trimester Ultrasound
Prenatal diagnosis, as practised today, relies on a long series of scientific advances. “In 1992, the British doctor of Cypriot origin, Nikolaides, was interested in nuchal translucency, a fluid-filled space between the skin and the spine visible on ultrasound at the level of the fetus’s neck. He realised that the thicker this space is between 11 and 14 weeks after the last menstrual period (weeks of amenorrhoea), the higher the risk of trisomy 13, 18 or 21.” To define the risk of chromosomal abnormalities per 1000, the gynaecologist also considers factors such as age. He also measures certain markers in the mother’s blood as early as 9 weeks (free β-hCG and PAPP-A).
For this nuchal translucency measurement, it is now more appropriate to perform an ultrasound around 12 weeks of amenorrhoea. In the past, this ultrasound was carried out later in Switzerland. Advances in equipment also enable the detection of certain malformations in the first trimester. “Ultrasound machines released in the last five years have impressive image quality,” says the specialist. “They allow us to see very small structures, even though the foetus moves a lot at this age. Certain malformations of the cardiac, nervous, or abdominal systems can, for example, be detected in 70-100% of cases. We proceed with an anatomical examination of the foetus, with results similar to those obtained only in the second trimester.”

The Invention of a Non-Invasive Test
Another major change in prenatal diagnosis was introduced in Switzerland ten years ago. When the risk of trisomy is considered high (from a probability of 1 in 380), or intermediate (from 1 in 1,000) following the first ultrasound and the tests explained above, mothers who wish it can have a "non-invasive prenatal test" (NIPT) reimbursed by health insurance. It is based on detecting foetal DNA in maternal blood, originating from an additional chromosome (13, 18 or 21). In 2023, more than 21,000 tests of this type were performed on patients followed in Switzerland, compared with about 19,000 in 2019, according to the FOPH. “As this is a screening, with its share of unknowns (false positives are in the order of 0.04% for trisomy 21), a positive result for one of these chromosomal abnormalities must be confirmed by an amniocentesis”. Joanna Sichitiu notes that this last invasive examination has become safer in recent years, thanks to increased ultrasound precision and the expertise of specialised obstetricians, leading to a decrease in the risk of miscarriage. “The introduction of the needle into the amniotic fluid by the obstetrician is always performed under ultrasound guidance.”
The National Advisory Commission on Biomedical Ethics (NCE) published a 2016 position paper on non-invasive prenatal testing and its practical implementation. “Prenatal screening techniques, such as DNA sequencing, continue to improve in accuracy”, says Markus Zimmermann, President of the NCE. “However, therapeutic or interventional options evolve more slowly. In many cases, as a parent, I can either accept the diagnosis and prepare for it so as not to be surprised at birth, or I can terminate the pregnancy. Given the significant share of false positives, it is important from an ethical point of view that a termination of pregnancy should not be carried out solely on the basis of an NIPT result.”
Preparing the Announcement to Parents
Improvements to prenatal screening required adaptations to gynaecology-obstetrics services and practices in Switzerland, including technical changes as well as the management of communication with parents. As Laure*, mother of a child with trisomy 21 (see box), pointed out, announcements of high risk of trisomy can come as a shock.
"At each step, we communicate the exam results to the parents in a transparent manner,” explains Joanna Sichitiu. “We try not to be alarmist, but we answer their questions honestly. Psychological support can also be arranged to accompany them through the diagnostic process. Some genetic tests can take up to a month, and this waiting period is very difficult for parents.”
To explain the diagnosed chromosomal abnormality, malformation, or complication, the CHUV organises a meeting between the parents and the specialists involved. “This prevents patients from being shuffled from one department to another. In the same room, for example, there can be a neonatologist to discuss the progress of care at birth, a surgeon to provide details of the operation on the affected part of the body, or even a geneticist to provide information on the genetic disease in question. The majority of parents do not want 'perfect babies', but ask us about the quality of life of the unborn child and whether it will suffer, especially in the case of malformations.”
For Dr Sichitiu, it is important to give space to parents who need time to think, for example, about a termination of pregnancy (therapeutic termination of pregnancy). Ruth Foley was indeed sorry to have been pushed to make a decision after the announcement of her daughter’s trisomy (see testimony in the box). Contact with patient organisations for those affected by the same malformations or chromosomal variations, as well as with their parents, can be useful in these situations. The Association Romande Trisomie 21 (ART 21), for example, offers to organise meetings with other parents who have discovered that their child has trisomy 21.
“We needed space to make our decision”

Ruth
“Pregnant with my second child, I underwent the first-trimester screening, which revealed a high probability of trisomy 21 and a potential for trisomy 18. After this announcement, the gynaecologist asked us to make a decision quickly, without giving us the space we needed to consider whether to continue with the pregnancy. The second gynaecologist we consulted was much more attentive. When I asked her, 'What would you do if you were me?’, she simply replied that she didn’t know and that she was there to help us, no matter our decision.
My husband and I needed more information and agreed to a non-invasive prenatal test, followed by an amniocentesis. The examination revealed that it was only a variation of chromosome 21. At the same time, we met a cardiologist because of a heart problem detected during the first ultrasound. She told us it was fixable and spent a lot of time with us, sharing stories of children with Down syndrome who had enriched her life.
Based on this information, we gave it a great deal of thought. We asked ourselves many questions: Can we welcome this child? What would be the impact on our eldest daughter of having a little sister with Down syndrome? We knew we would face many medical appointments and challenges related to inclusion at school and in society, as well as how others view us. Still, it is always difficult to anticipate the impact a child will have on your life, even when they are born without a disability. Despite being two to raise her and without financial problems, it was our long-standing commitment to an inclusive society that ultimately guided our decision. As with all children, there are good days and more difficult ones. Our daughter has made our whole family better; she has expanded our horizons.
Laure*
“A few days after the first ultrasound, my gynaecologist explained to me over the phone that there was a 1 in 8 chance the foetus had trisomy 21 and a one in 170 chance it had trisomy 13 or 18. I was in shock; I did not expect it at all.
Since my husband and I wanted to know more about the child’s viability, we agreed to a chorionic villus sampling (an invasive procedure that involves collecting micro-fragments from the placenta, called chorionic villi). We were in a difficult period of waiting for the test results, filled with intimate reflections as a couple. Being surrounded by our loved ones, without receiving advice, was very valuable. It is a very personal decision, and only the parents go on to live with the child with a trisomy or with an abortion.
During this period of doubt, I remembered a family I followed on social media who had adopted a child with Down syndrome. I had been lifted by their testimony, by this unconditional love, and by the joy one could also find in disability. I contacted them, which helped us along our journey with trisomy until our appointment with the geneticist.
The CHUV geneticist had analysed the chorionic villus sampling results. We asked her to tell us the baby’s gender first, because we wanted to personalise and humanise the child. It was a boy, and I told him we were going to call him Louis*. 'Louis has trisomy 21,' she simply said. We then asked her, ‘Many people are afraid for the rest of our family life; they do not necessarily understand why we wish to keep this child. You’ve been a geneticist for years. What do you think?’ She took her time before responding: ‘I believe that this world needs these differences. And when a family prepares as you have, things generally go very well.’
We were followed by excellent doctors. The cardiologist took the time to explain to us how Louis would be operated on for his heart condition at four months old, and that I would be able to spend an hour with him at his birth before he was taken for the necessary examinations. When the day came, meeting Louis dispelled all our previous fears. He is a joyful, full-of-life child who progresses well in his therapies at his own pace. He teaches us a lot and enriches our family. Trisomy ultimately becomes just a characteristic; it does not define the whole person.
Today, I am involved with ART 21 to connect parents in similar situations. I also help develop the 'First Steps' kits offered to mothers who have just given birth, so that every birth is celebrated.
*Pseudonym
Second-Trimester Diagnosis
While many pathologies or abnormalities are discovered in the first trimester, others are only detected during the second ultrasound. This is often the case, for example, with neural tube defects called 'spina bifida' or an anomaly of the corpus callosum (the absence or incomplete development of the bridge that connects the two hemispheres of the brain). If the legal period for voluntary termination of pregnancy (IVG) in Switzerland, of 12 weeks of amenorrhea, is exceeded and the mother wishes to terminate the pregnancy, a medical opinion must demonstrate the necessity of the interruption to eliminate the danger of serious bodily harm to the mother or a state of deep distress of the pregnant woman. “The danger will be all the more serious as the pregnancy has progressed”, according to the law. “At the CHUV, we accompany and inform patients,” says Joanna Sichitiu. “Then, an ethics committee, which may include several specialists (obstetrician, neonatologist, paediatrician, geneticist, ethicist, caregiver, psychiatrist, lawyer, etc.), meets to respond to the request. If the committee objects, patients can seek treatment at another university centre or abroad. However, these situations remain exceptional.”
The National Advisory Commission on Biomedical Ethics (NCE) published a position paper in 2018 on screening at an advanced stage of pregnancy and the possibility of interruption during this period. “After listening to 16 experts on the subject, we came to the conclusion that the current regulations were judicious,” explains its president. “The Swiss penal code, in Article 119, stipulates that an abortion may be performed until birth. But the later it is performed, the more serious the attack on the life of the person concerned must be in case of continuation of the pregnancy. Indeed, the embryo's development at the time of the second ultrasound is much more advanced than during the first, which represents an important ethical shift. The foetus is usually able to survive outside the uterus from 22 weeks of gestation.”
From an ethical standpoint, the essential task is to offer "the best possible personal support in this situation," according to the professor of theology at the University of Fribourg. “It is important that the medical profession be prepared to sit down and discuss at length with the parent(s) what a particular outcome means. Translating technical language for parents by adapting to their knowledge and representations is crucial. Patients expecting their first child, for example, will not necessarily share the same vision as those who already have three.” This requires time and is a challenge to be taken all the more seriously, as the rising age of mothers in Switzerland could make these situations more frequent.
“An exciting breakthrough for mothers”
Early detection of preeclampsia is an "exciting breakthrough for mothers," says Dr Joanna Sichitiu of the CHUV. This disease affects about 2% of pregnancies, and its most serious maternal complication, eclampsia (convulsions), accounts for about 10% of maternal deaths in Asia and Africa and 25% in Latin America, according to the World Health Organisation. It also leads to complications for the foetus, such as extreme premature birth and growth delays. “Preeclampsia was previously monitored mainly by assessing symptoms such as tinnitus and visual changes. Recently, it has become possible to identify patients at risk during the first-trimester ultrasound by analysing vascular resistance in the visible uterine arteries. The new algorithm also takes into account maternal factors such as age and obstetric background, as well as the mother’s blood pressure and a protein in her blood called placental growth factor.” Thanks to this screening, pregnant women can be better monitored for the rest of their pregnancy and receive aspirin-based treatment that will reduce the risk of developing preeclampsia by up to 70%.


![[Translate to Anglais:] ©Large Network](https://www.invivomagazine.ch/fileadmin/_processed_/6/8/csm_LN_INVIVO_HOPITAL-FUTUR_MINIATURE_MINIATURE_337551332d.jpg)
